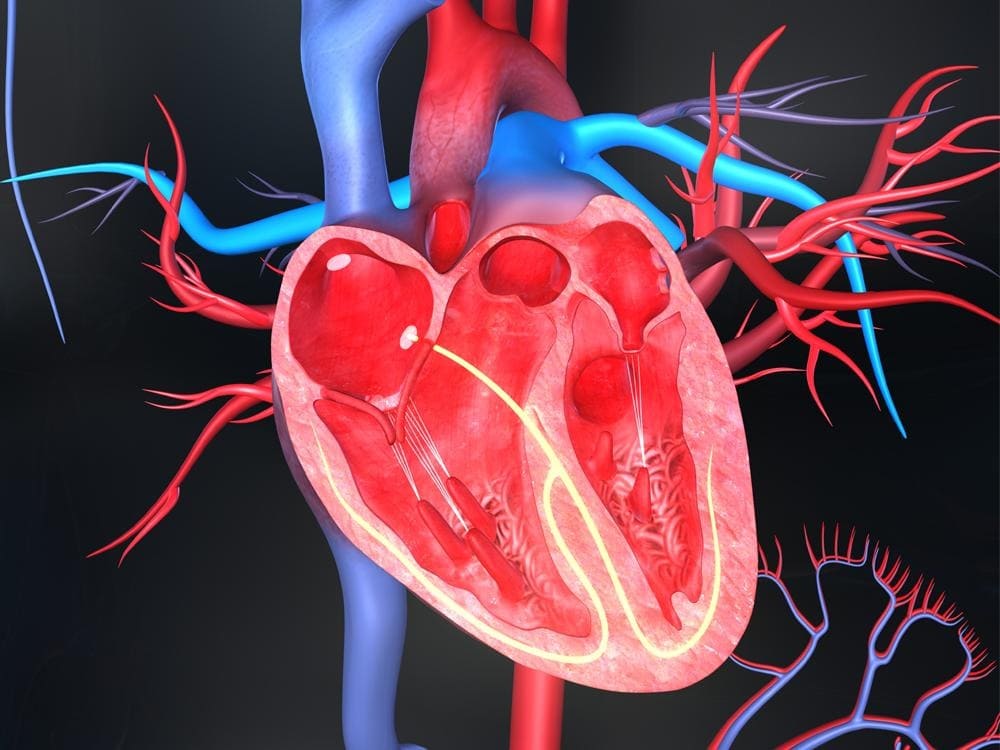
Structural heart disease refers to abnormalities in the heart’s anatomy that are present at birth (congenital) or develop later in life. These abnormalities affect the structure of the heart and the way blood flows through it. Structural heart defects are relatively common, affecting nearly 1% of the population. Many structural heart diseases can be effectively treated with surgery or medical procedures to repair or replace defective parts of the heart.
What is Structural Heart Disease?
Structural heart disease includes a range of congenital (present at birth) and acquired abnormalities that affect the heart’s shape or function. Some examples of structural heart diseases include:
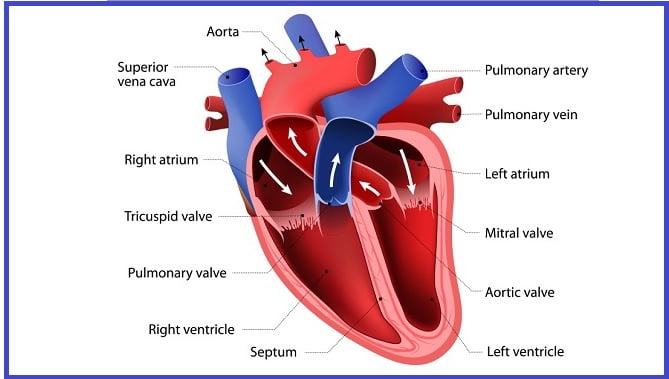
- Congenital heart defects – These are problems with the heart’s structure that are present at birth. Examples include holes in the heart (septal defects), narrowing of valves or blood vessels, and abnormal positioning of arteries and veins. Congenital heart defects affect nearly 1% of births.
- Valvular heart disease – This involves dysfunction of one of the four heart valves. It can be present at birth or develop later in life due to wear and tear, infection, or other causes. Examples are aortic stenosis (narrowing of the aortic valve) and mitral regurgitation (leaking of the mitral valve).
- Cardiomyopathy – This refers to diseases of the heart muscle that make it harder for the heart to pump blood effectively. The heart may become enlarged, thick, or rigid. Types include dilated, hypertrophic, and restrictive cardiomyopathy.
- Aortic aneurysms or dissections – This involves abnormal enlargement or splitting of the aorta, the major blood vessel that carries blood from the heart. This can prevent proper blood flow and requires urgent repair.
- Atrial septal defects – This congenital heart defect involves a hole in the wall (septum) between the heart’s two upper chambers (atria). This allows blood to leak between the atria.
- Ventricular septal defects – Also a congenital defect, this involves a hole in the wall between the heart’s two lower chambers (ventricles). This can cause oxygen-rich and oxygen-poor blood to mix.
Symptoms of Structural Heart Disease
The symptoms of structural heart disease depend on the specific defect or abnormality. Some common signs and symptoms include:
- Shortness of breath – Especially during physical activity or exercise
- Fatigue or tiredness
- Swelling in the legs, feet, or abdomen
- Palpitations or irregular heartbeat
- Fainting or dizziness
- Chest pain or tightness
- Cyanosis – A bluish tint to the skin, lips, and nails
- Poor feeding and failure to thrive in infants
Some congenital heart defects may not cause noticeable symptoms until adulthood. Others can be life-threatening soon after birth if the defect severely impacts blood circulation. Symptoms that appear suddenly or worsen rapidly often require prompt medical care.
Causes and Risk Factors
Congenital Heart Defects
Congenital heart defects develop in utero when the heart is forming during fetal development. The exact causes are often unknown but may involve:
- Genetic factors – Defects in certain genes can disrupt normal heart development. Many congenital heart diseases run in families.
- Environmental factors – Smoking, alcohol use, some medications, and viral infections during pregnancy may increase the risk.
- Multifactorial – Interactions between genes and the environment likely play a role.
Acquired Structural Heart Diseases
These abnormalities arise later in life. Contributing factors can include:
- Diseases or infections – Conditions that affect heart health like coronary artery disease, high blood pressure, rheumatic fever, endocarditis, and cardiomyopathy can alter the shape and function of heart structures.
- Aging and wear-and-tear – Years of constant heartbeat can fatigue heart valves, causing leakage, stenosis, or prolapse.
- Injuries – Physical trauma, radiation exposure, or damage from a heart attack can impair the heart.
- Medications – Certain chemotherapy drugs, antidepressants, and appetite suppressants have been linked to valvular disease and aortic aneurysms.
- Lifestyle factors – Smoking, excessive alcohol use, and obesity contribute significantly to acquired structural heart problems.
Diagnosing Structural Heart Disease
Diagnosing structural heart disease often begins with a physical exam, medical history, and noticing any symptoms. Some common diagnostic tests include:
- Echocardiogram – This ultrasound creates images of the heart’s anatomy and detects abnormalities. It is typically the first test ordered if heart disease is suspected.
- Electrocardiogram – Records the heart’s electrical signals and can detect arrhythmias, heart enlargement, and ischemia.
- Chest x-ray – Provides images that may reveal an enlarged heart or fluid buildup in the lungs.
- Cardiac catheterization – A long thin tube is threaded into the heart to inject dye and visualize the arteries and heart chambers under x-ray imaging.
- MRI or CT scan – Provides detailed 3D images of the structure of the heart and major blood vessels.
- Genetic testing – Identifies abnormalities in genes associated with congenital heart defects.
Depending on the results, additional tests such as a stress test, cardiac CT or MRI, or heart biopsy may be ordered. Newborn infants are screened for critical congenital heart disease with pulse oximetry testing.
Treatment Options for Structural Heart Disease
Treatment options depend on the type and severity of the structural defect. They aim to relieve symptoms, prevent complications, and improve quality of life. Options may include:
Medications
- Blood thinners – Used to prevent clotting and stroke if heart structures are malformed. Includes warfarin, heparin, and aspirin.
- ACE inhibitors or ARBs – help relax blood vessels and lower blood pressure. Used for cardiomyopathy, and septal defects.
- Beta-blockers – Helps control abnormal heart rhythms and high blood pressure.
- Diuretics – Eliminate fluid buildup in the lungs and peripheral edema.
- Digoxin – Improves heart function and manages certain arrhythmias like atrial fibrillation.
- Antiarrhythmics – Helps maintain normal sinus rhythm for arrhythmias.
Medical Procedures
- Cardiac catheterization – Can close septal defects, repair or replace valves, or widen narrow arteries.
- Balloon valvuloplasty – Uses a catheter to insert a balloon that opens up a narrowed heart valve.
- Coronary angioplasty – Opens clogged coronary arteries that may contribute to structural disease.
- Implantable devices – Includes pacemakers, defibrillators, and cardiac resynchronization devices. Manages arrhythmias.
- Heart transplant – For end-stage heart failure when other treatments have failed. Replaces the diseased heart.
Surgery
- Open heart surgery – Repairs or replaces defective heart valves and corrects septal defects, arrhythmias, aneurysms, etc. Requires cardiopulmonary bypass.
- Minimally invasive heart surgery – Uses small incisions and robotic assistance to fix certain structural defects. Shorter recovery than open surgery.
- Ventricular assist devices (VADs) – Mechanical pumps that support heart function and blood flow for failing hearts. Can be permanent or short-term until transplant.
New and Emerging Treatments
Advances are continually being made in treating structural heart disease. Some newer approaches include:
- Transcatheter valve replacements – Valves can now be implanted via catheter through a small incision rather than opening the chest. Less invasive than surgery.
- 3D-printed heart models – Allows surgeons to prepare and practice procedures on a replica of the patient’s heart anatomy. Leads to better outcomes.
- Gene editing – Technologies like CRISPR show promise for repairing genetic defects that cause congenital heart disease before birth. Still experimental.
- Stem cell therapy – Cells injected into damaged heart muscle may be able to improve healing after a heart attack or help restore cardiac function. Currently being researched.
- CorMatrix ECM technology – Acellular collagen matrix can help repair heart defects and regenerate tissue during procedures. Showing positive results.
- Nanotechnology – Microscopic particles and mesh can deliver medications directly to areas of structural disease. May allow less invasive treatments.
Continuing research brings hope for less invasive and more targeted treatments for structural heart conditions in the future. Patients should ask their doctor about clinical trials they may qualify for.
Living with Structural Heart Disease
Although many structural defects require invasive surgery to repair, other types may be managed effectively with lifestyle changes and careful monitoring. Some tips for living well with structural heart disease include:
- Take all medications as prescribed. Don’t stop or change the dose without consulting a doctor.
- Attend regular follow-up visits to monitor for changes in symptoms or heart function. Report new symptoms promptly.
- Restrict sodium to minimize fluid retention which can worsen heart failure symptoms. Follow diet recommendations.
- Limit alcohol intake, as heavy drinking makes structural disease and heart failure worse.
- Stop smoking, maintain a healthy weight, and stay active. Aerobic exercise helps, but check limits.
- Manage stress levels and practice relaxation techniques. Avoid triggers that cause palpitations or chest pain.
- Use home blood pressure monitoring and adjust medications to keep levels in target range.
- Carry emergency medical ID describing heart conditions and medications. Seek help immediately for serious symptoms.
- Join a support group to share experiences and helpful tips for living with heart disease.
Pregnancy requires special care – check with the obstetrician and cardiologist about any risks. Report concerning symptoms right away. Address mental health conditions like anxiety or depression that often accompany chronic disease. Most patients will need to limit high-intensity activities but can lead fulfilling lives by effectively managing their structural heart condition.
FAQs
What is the life expectancy for someone with structural heart disease?
Life expectancy varies greatly depending on the specific defect, its severity, and how well it can be repaired. Structural problems that cause heart failure can significantly impact life expectancy if not treated. However, certain defects like small septal defects may cause minimal complications. Patients should speak with their cardiologist about the prognosis.
How are congenital heart defects diagnosed prenatally?
Ultrasounds and fetal echocardiograms during pregnancy can often detect major structural abnormalities before birth. Additional specialized tests like fetal MRI may help confirm findings. Genetic testing can also identify congenital defects. Diagnosis allows parents to plan for treatment soon after delivery.
Can structural heart defects develop in adults?
Yes, some types of valvular disease, cardiomyopathy, and aneurysms occur only in adults due to cumulative wear and tear, health conditions, or aging. Heart attacks and radiation therapy also sometimes cause structural damage later in life. Regular cardiac checkups help detect acquired disease early.
What is the best treatment for an enlarged heart (dilated cardiomyopathy)?
Along with medications to improve heart function, implanted devices like CRT and ICD are often used. A ventricular assist device may support the heart while awaiting a transplant. For end-stage failure, a heart transplant is currently the only definitive treatment. Lifestyle changes like diet, exercise, and stopping alcohol are key.
How successful is transcatheter aortic valve replacement versus open heart surgery?
For patients with aortic stenosis, TAVR is equally effective as surgery with shorter recovery times. Approval has expanded to lower-risk patients. The choice depends on multiple patient-specific factors. Discuss both options thoroughly with a cardiothoracic surgeon.
Conclusion
Structural heart defects, both congenital and acquired, affect the heart’s normal anatomy and function. Thanks to major treatment advances, many structural diseases that were once fatal can now be repaired or managed effectively. Options range from medications and minimally invasive procedures to open heart surgery and transplants. Continuing research promises even less invasive options in the future. With appropriate treatment guided by cardiac specialists, patients with structural heart disease can often live active, full lives. Staying adherent with follow-up care is key to detecting changes and achieving the best possible long-term outcomes.
Mustafa Al Mahmud is a passionate medical writer and health enthusiast. He is excited to share his knowledge and make reliable health information more accessible through Quick Medico. Mustafa aims to write about common diseases, medications, wellness topics, and the latest health research in easy-to-understand language. He believes clear and accurate health communication empowers readers to take charge of their well-being. In his free time, Mustafa enjoys hiking, cooking, and spending time with his family.